Maternal mortality, a critical indicator of health system effectiveness, continues to plague the United States, which unfortunately leads high-income nations in pregnancy-related deaths. Recent studies underscore that an alarming number of these fatalities, over 80%, are preventable with improved prenatal and postpartum care. The upward trend in maternal mortality rates between 2018 and 2022 highlights significant health disparities linked to state, race, and ethnicity. High-risk pregnancies are a contributing factor to this crisis, further necessitating robust maternal health care policies that can effectively target inequalities across different demographics. Addressing the root causes of postpartum mortality and the social determinants of health is essential in reversing this trend and ensuring that every mother has the opportunity for a safe birthing experience.
The term maternal mortality can sometimes be understood through varied phrases like pregnancy-associated deaths or maternal fatalities. These terms reflect the serious issue of mortality rates among women during and after childbirth, particularly in circumstances deemed high-risk. Despite advancements in medical science, challenges surrounding maternal health care persist, leading to alarming rates of postpartum mortality within vulnerable populations. Inequities in access to care exacerbate health disparities, making it imperative for communities and policymakers to focus on comprehensive strategies aimed at improving maternal outcomes. By exploring the complexities of this issue, we can begin to unravel the systems that contribute to these devastating statistics and advocate for necessary changes.
Understanding Maternal Mortality in the U.S.
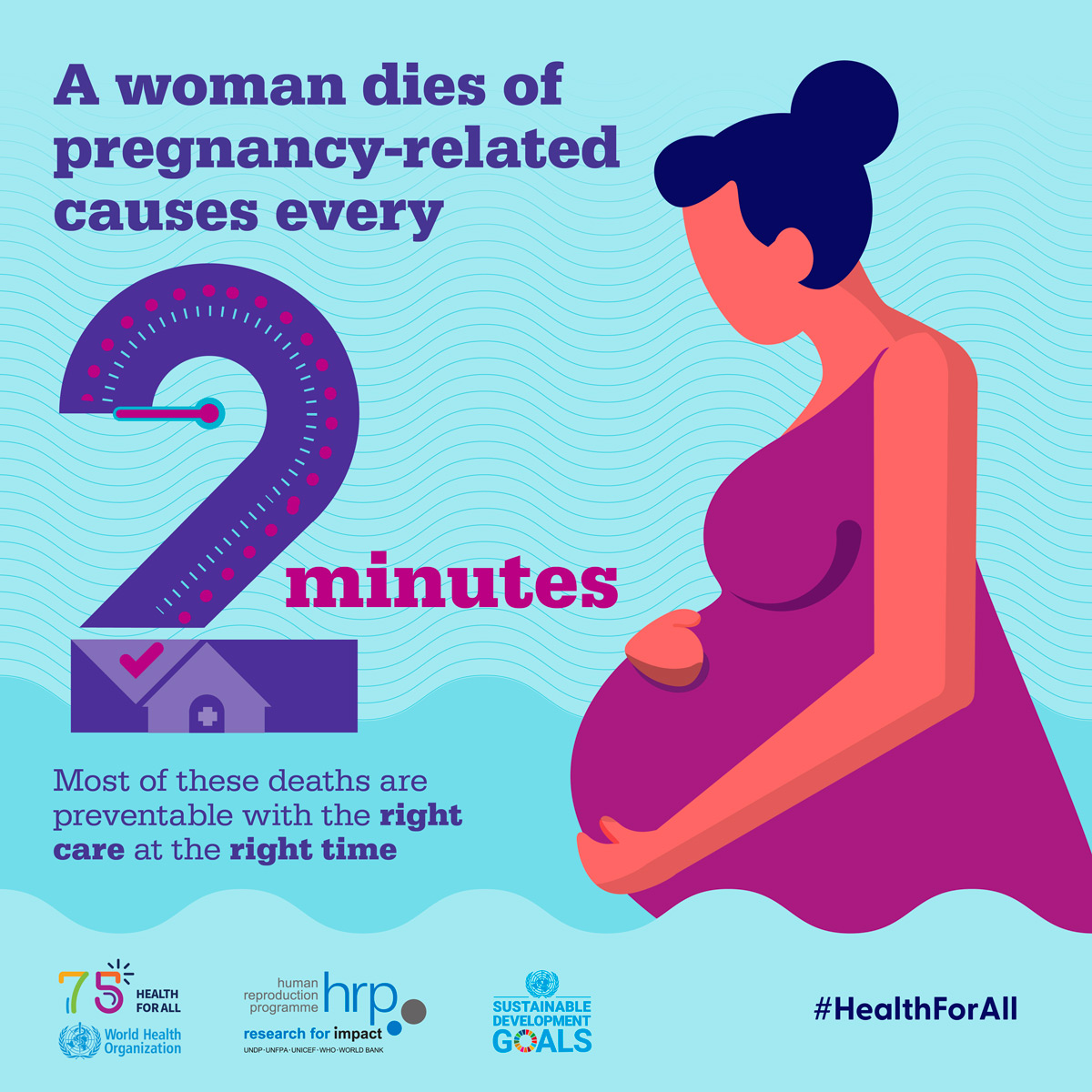
Maternal mortality remains a critical public health issue in the United States, as the nation lags behind its high-income peers with rising rates of pregnancy-related deaths. The statistics are alarming, with the maternal mortality rate consistently increasing from 2018 to 2022, highlighting a significant public health crisis that requires immediate attention. Despite advancements in medical technology and healthcare, more than 80% of pregnancy-related deaths are identified as preventable. This troubling reality emphasizes the need for comprehensive maternal health care solutions, encompassing both prenatal and postpartum care, to effectively address the factors contributing to these deaths.
The persistence of high maternal mortality rates can be attributed to various systemic issues, including inadequate access to maternal health care, which disproportionately affects marginalized communities. The disparity in maternal health outcomes among racial and ethnic groups is notable, as American Indian and Alaska Native women experience mortality rates nearly four times higher than white women. Such health disparities underscore the urgent necessity for targeted interventions to improve maternal health care systems across the country, ensuring equitable access for all individuals regardless of race or socioeconomic status.
The Role of Health Disparities in Maternal Health
Health disparities play a significant role in the rising maternal mortality rates observed in the U.S., contributing to unequal access to essential health services. Women of color, particularly American Indian, Alaska Native, and African American women, face elevated risks due to a combination of socioeconomic factors, inadequate healthcare infrastructure, and systemic discrimination. Addressing these disparities is essential for improving maternal health outcomes. Efforts must be focused on reforming health policies, enhancing community-based support systems, and increasing awareness around the unique challenges faced by high-risk pregnancies.
Furthermore, understanding the underlying social determinants of health, such as education, income, and availability of healthcare resources, is crucial in identifying effective strategies to reduce health disparities. Policies aimed at improving maternal health care must prioritize comprehensive services that cater to the specific needs of diverse populations, ensuring that no woman is left behind in her journey through pregnancy and postpartum recovery. Fostering collaboration between healthcare providers and community organizations will be vital in creating a more inclusive health care landscape.
The Impact of Cardiovascular Disease on Maternal Health
Cardiovascular disease has emerged as the leading cause of pregnancy-related death in the United States, accounting for over 20% of maternal fatalities. This shift in primary causes for maternal mortality underscores the urgent need for increased awareness surrounding the risks associated with chronic health conditions during and after pregnancy. Women of reproductive age are increasingly experiencing chronic issues like hypertension, signaling a worrying trend of cardiovascular risk factors affecting younger populations. The recognition of these trends is crucial for developing targeted interventions that can reduce the incidence of cardiovascular complications in pregnancy.
In response to this alarming trend, healthcare providers must adopt a proactive approach by integrating cardiovascular risk assessments into routine prenatal care. This involves early identification and management of high-risk pregnancies, as well as tailored care plans that specifically address the cardiovascular health of pregnant individuals. By prioritizing cardiovascular health within the realm of maternal care, we can significantly mitigate the risks associated with pregnancy-related deaths and enhance the overall health outcomes for mothers and their newborns.
Addressing Postpartum Mortality: A Comprehensive Approach
Postpartum mortality, particularly late maternal deaths occurring between 42 days to one year after childbirth, highlights a significant gap in maternal health care in the U.S. Traditionally, the definition of maternal mortality has focused on deaths occurring within 42 days postpartum, neglecting the extended recovery period which is critical for maternal health. As studies indicate that nearly one-third of maternal deaths occur post-42 days, there is a compelling need for healthcare systems to expand their focus beyond the immediate postpartum period to address ongoing health needs.
To effectively tackle postpartum mortality, comprehensive health care strategies should be implemented that acknowledge this extended timeline. This includes enhanced access to mental health services, ongoing medical assessments, and support for chronic health issues that may arise during the postpartum phase. By treating the postpartum period as a continuum rather than a discrete phase, healthcare providers can better monitor and support new mothers, ultimately reducing preventable deaths and improving long-term health outcomes.
The Importance of Data in Maternal Health Research
Effective maternal health policies require a solid foundation of data and research to identify and address the complexities surrounding maternal mortality. Since the implementation of tracking measures such as the pregnancy checkbox on death certificates in 2018, a clearer picture of maternal deaths has emerged. This advancement is crucial in addressing the gaps in understanding maternal health outcomes, as consistent data collection allows researchers to identify patterns, risk factors, and disparities that affect maternal health across different demographics.
Moreover, ongoing research initiatives must focus on building a comprehensive database of maternal health outcomes that captures the diverse experiences of women across the United States. By leveraging this data, policymakers can develop informed strategies that target the root causes of maternal mortality and health disparities. This proactive approach in maternal health research is vital for driving systemic changes that prioritize women’s health and ensuring that actionable insights lead to improved maternal health care standards.
Advances in Maternal Health Care Practices
Advancements in technology and health care practices hold promising potential for reducing maternal mortality rates. Innovations in telehealth and remote monitoring, for instance, have made it easier for pregnant individuals to receive timely care and support from healthcare providers. This is especially critical in underserved areas where access to quality maternal health services may be limited. By integrating modern technology into maternal health care, healthcare systems can enhance monitoring and early intervention, ultimately leading to better health outcomes for mothers.
Additionally, educational programs aimed at expecting mothers about the warning signs of complications during pregnancy and the postpartum period can empower women to seek help earlier. These proactive measures, combined with advanced care practices, can substantially mitigate the risks associated with high-risk pregnancies, consequently leading to a decline in maternal mortality rates. The integration of technology along with patient education represents a transformative approach to maternal health that prioritizes safety and well-being.
Promoting Health Equity in Maternal Care
Promoting health equity within maternal care is crucial to ensuring that all women receive the support and services they need during pregnancy and postpartum. Addressing the disparities faced by racial and ethnic minorities requires a multi-faceted approach that tackles the underlying social determinants of health. Initiatives aimed at improving economic stability, access to education, and healthcare resources are essential in creating a more equitable healthcare landscape for all pregnant individuals, regardless of background.
By emphasizing culturally competent care and involving community leaders in maternal health initiatives, healthcare providers can better serve diverse populations. Developing inclusive policies that recognize and address the unique challenges faced by high-risk groups will be instrumental in reducing maternal mortality rates. This commitment to health equity not only improves outcomes for women but also fosters a healthier future for their children and communities.
Future Directions for Maternal Health Policies
The future of maternal health policies must prioritize proactive investment in public health infrastructure to combat rising maternal mortality rates. Policymakers are challenged to address the systemic inequities that contribute to disparate outcomes while also enhancing access to quality care. This requires a concerted effort to implement innovative solutions tailored to the unique needs of different populations, particularly those at high risk for maternal mortality.
Furthermore, collaboration across various sectors—healthcare, education, and community organizations—will be critical in shaping effective maternal health policies. By fostering partnerships that aim to enhance care delivery and access to resources, we can create a comprehensive framework that supports pregnant individuals throughout their journey. Continued focus on maternal health, including addressing postpartum support and improving the quality of care, will be essential in reversing the trend of rising maternal mortality rates.
Building Collaborative Care Models in Maternal Health
Developing collaborative care models in maternal health is vital for addressing the multifaceted challenges that contribute to high maternal mortality rates. Such models promote teamwork among healthcare professionals from various disciplines, including obstetricians, midwives, mental health specialists, and community health workers. By working collaboratively, these professionals can provide integrated care that meets the diverse needs of pregnant individuals, facilitating timely interventions and comprehensive support.
Furthermore, engaging patients in their care through shared decision-making processes empowers them to take an active role in their health. Collaborative care underscores the importance of holistic approaches that encompass both physical and mental wellness, which could significantly reduce risks associated with high-risk pregnancies. By prioritizing collaboration in maternal health care, we can create more supportive environments that prioritize the well-being of mothers and their families.
Frequently Asked Questions
What are the key factors contributing to the high maternal mortality rate in the U.S.?
The high maternal mortality rate in the U.S. is influenced by various factors including a fragmented healthcare system, health disparities across racial and ethnic groups, and increasing prevalence of chronic conditions like cardiovascular disease among individuals of reproductive age. Inequitable policies and maternity care deserts also play a significant role in this public health crisis.
How do health disparities impact pregnancy-related deaths in the United States?
Health disparities significantly impact pregnancy-related deaths in the United States. Certain racial groups, such as American Indian and Alaska Native women, experience mortality rates nearly four times higher than white women. This discrepancy highlights the urgent need for policy changes and targeted maternal health care to address underlying inequalities in access and quality of care.
What is the significance of postpartum mortality in maternal health discussions?
Postpartum mortality, which refers to deaths occurring between 42 days and one year after childbirth, is crucial in maternal health discussions because it represents a significant portion of pregnancy-related deaths. Acknowledging this time frame encourages healthcare systems to provide comprehensive postpartum care and recognize recovery as an ongoing process rather than a finite period.
Why should late maternal deaths be included in the conversation about maternal mortality?
Late maternal deaths should be included in conversations about maternal mortality because they account for a substantial number of deaths related to pregnancy. By expanding the definition of maternal mortality to include deaths occurring up to one year postpartum, healthcare systems can better address ongoing maternal health needs and improve support during the critical recovery phase.
What measures can be implemented to reduce maternal mortality rates in high-risk pregnancies?
To reduce maternal mortality rates in high-risk pregnancies, measures such as enhancing access to quality maternal health care, increasing prenatal check-ups, improving education on chronic conditions, and addressing systemic biases in healthcare must be prioritized. Additionally, investments in public health infrastructure and tailored programs for vulnerable populations can create more equitable outcomes in maternity care.
How does the COVID-19 pandemic relate to the increase in maternal mortality rates?
The COVID-19 pandemic has been linked to an increase in maternal mortality rates, especially during its onset in 2020. The stress on the healthcare system, lack of resources, and disruptions in routine prenatal and postpartum care contributed to worsening outcomes for pregnant individuals, as evidenced by a sharp rise in mortality rates observed in 2021.
What role does cardiovascular disease play in pregnancy-related deaths?
Cardiovascular disease is the leading cause of pregnancy-related deaths, accounting for over 20% of such fatalities. The increasing prevalence of conditions like hypertension and cardiovascular disorders among younger individuals of reproductive age indicates a need for heightened awareness and management of these health issues during and post-pregnancy.
What steps can we take to improve maternal health care and reduce mortality rates?
Improving maternal health care and reducing mortality rates can be achieved by investing in health infrastructure, addressing state-level health disparities, offering comprehensive prenatal and postpartum services, and fostering community support systems. Enhanced research funding and policies focusing on equitable access to quality care are essential for improving maternal health outcomes.
| Key Point | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income nations, with a rise noted from 25.3 to 32.6 deaths per 100,000 live births between 2018 and 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable, indicating a need for improved healthcare interventions. |
| Racial Disparities | American Indian and Alaska Native women experienced the highest mortality rate of 106.3 deaths per 100,000 live births. |
| Impact of COVID-19 | The COVID-19 pandemic likely contributed to a sharp rise in maternal mortality in 2021, highlighting the intersection of public health and maternal health. |
| Chronic Conditions | Rising rates of chronic conditions like hypertension among younger individuals are influencing the rates of maternal mortality. |
| Late Maternal Deaths | Late maternal deaths accounted for nearly a third of total deaths, emphasizing the need for extended postpartum care. |
| Investment in Public Health | There is an urgent need for increased investment in public health infrastructure to address worsening maternal mortality rates. |
Summary
Maternal mortality remains a critical issue in the United States, with the country experiencing consistently high rates compared to other wealthy nations. This is particularly concerning as more than 80% of these deaths are preventable. The rising maternal mortality rates highlight the need for comprehensive healthcare reforms, improved prenatal and postpartum care, and targeted interventions to address racial disparities and chronic health conditions. Continued investment in public health infrastructure and innovative solutions is essential to reverse the current trends and ensure the safety of mothers during and after pregnancy.